New Culture System Could Lead to Developments in Pancreas Regeneration Studies
Typically, studies in cell and tissue regeneration processes make use of cultured cells that will be further observed. However, in the case of the pancreas, the cells rapidly disintegrate when placed in cultures due to self-digestion and lack of simultaneous oxygenation. This fact has limited scientists when conducting studies on the regeneration of the organ, which would be extremely helpful in the diagnosis and treatment of diabetes.
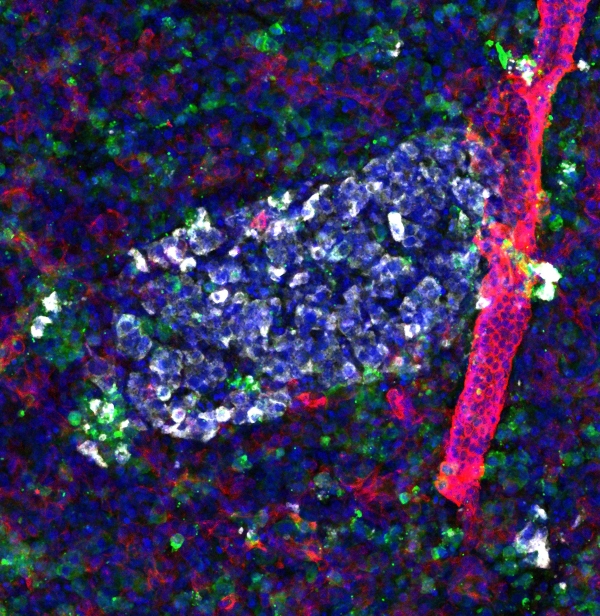
In a recently published study, scientists from the Diabetes Research Institute, or DRI, at the University of Miami Miller School of Medicine have found a way to allow long-term cultures of pancreatic slices that contain the cellular architecture and function of the pancreas in very thin sections. This then allows for further understanding of how the organ regenerates and replenishes insulin-producing beta cells over time.
In Vitro Setting Mimics the Natural Process
Scientists from the DRI made use of a culture system that was specifically designed to mimic the natural process of oxygenation in the pancreas. The setup has demonstrated, for the very first time, retained functionality in the human pancreatic slices, or HPSs, for a minimum of ten days from slicing.
Because of this, the researchers were able to quantify the formation of insulin-producing cells in HPSs from both non-diabetic and type 2 diabetic donors. The study focused on a population of stem-like "progenitor" cells which were observed to reproduce and give rise to insulin-producing beta cells in response to a natural growth factor, BMP-7.
From here, future studies of the pancreas that would make use of this in vitro setup could yield more accurate results. This is in comparison with studies involving preclinical work in animals.
Preservation of the Cytoarchitecture of the Pancreas: a 'Technical Breakthrough'
The DRI team used a culture device that improved the oxygenation of the cells, extending their life, structure, and function. The study's principal investigator, Dr. Juan Domínguez-Bendala, who is also the Director of Stem Cell Development for Translational Research and Research Associate Professor of Surgery at the DRI, has called the development a 'technical breakthrough':
"The ability to keep human pancreatic slices alive for nearly two weeks is a technical breakthrough that allows us to witness the regeneration of beta cells in a human model that strongly resembles the real pancreas," said Dr. Domínguez-Bendala. "We now have a window into the native human organ that simply wasn't possible prior to this study."
Research Professor of Medicine, Immunology, and Microbiology and the Director of the Molecular Biology Laboratory at the DRI, Ricardo Pastori, Ph.D., explained that this development is vital to going further with research on the regeneration of pancreatic cells. "Extending the life of these slices in culture was key to observe beta cell regeneration in real-time following the addition of BMP-7, even in slices obtained from diabetic donors," he said. "This gives us hope that we may be able to apply this approach to living patients one day."
READ NEXT: Bioprinted Skin Patches for Diabetic Foot Ulcers, Now Commercially Available
Jul 09, 2020 10:52 AM EDT